In the UK, we are seeing an increased number of cases of Group A streptococcus (Strep A) compared to normal at this time of year. Parents are being urged to be alert for the signs of Strep A infections. This is also known Group A streptococcal (GAS) or invasive Group A streptococcal (iGAS) infections.
Especially in winter, there are a range of causes of sore throats, colds and coughs caused by viruses that will get better by themselves without needing antibiotics or medical intervention, meaning it not being necessary to contact your GP surgery.
Occasionally, Strep A can lead to more serious illnesses like scarlet fever and, albeit rarely, very serious disease such as sepsis, Pneumonia or bone infections.
Across Yorkshire there has been an increase in cases this year, particularly in children under 10. Nationally, there have sadly been some deaths. We want parents to know what to look out for and when to seek medical care.
- If your child has a fever, sore throat, or fine red or pink rash that feels rough (like sandpaper) read our advice below.
- If your child seems more unwell than usual or if your child is getting worse or this illness is different to their normal coughs and colds, please seek medical attention.
What to do if you suspect your child has scarlet fever
Scarlet fever mainly affects children under 10, but people of any age can get it. In the early stages, symptoms include a sore throat, headache, and fever, along with a fine, pinkish or red body rash with a sandpapery feel. On darker skin, the rash can be more difficult to detect visually but will have a sandpapery feel.
We are asking parents to contact their GP if they suspect their child has scarlet fever, because early treatment with antibiotics is important to reduce the risk of complications such as pneumonia or a bloodstream infection.
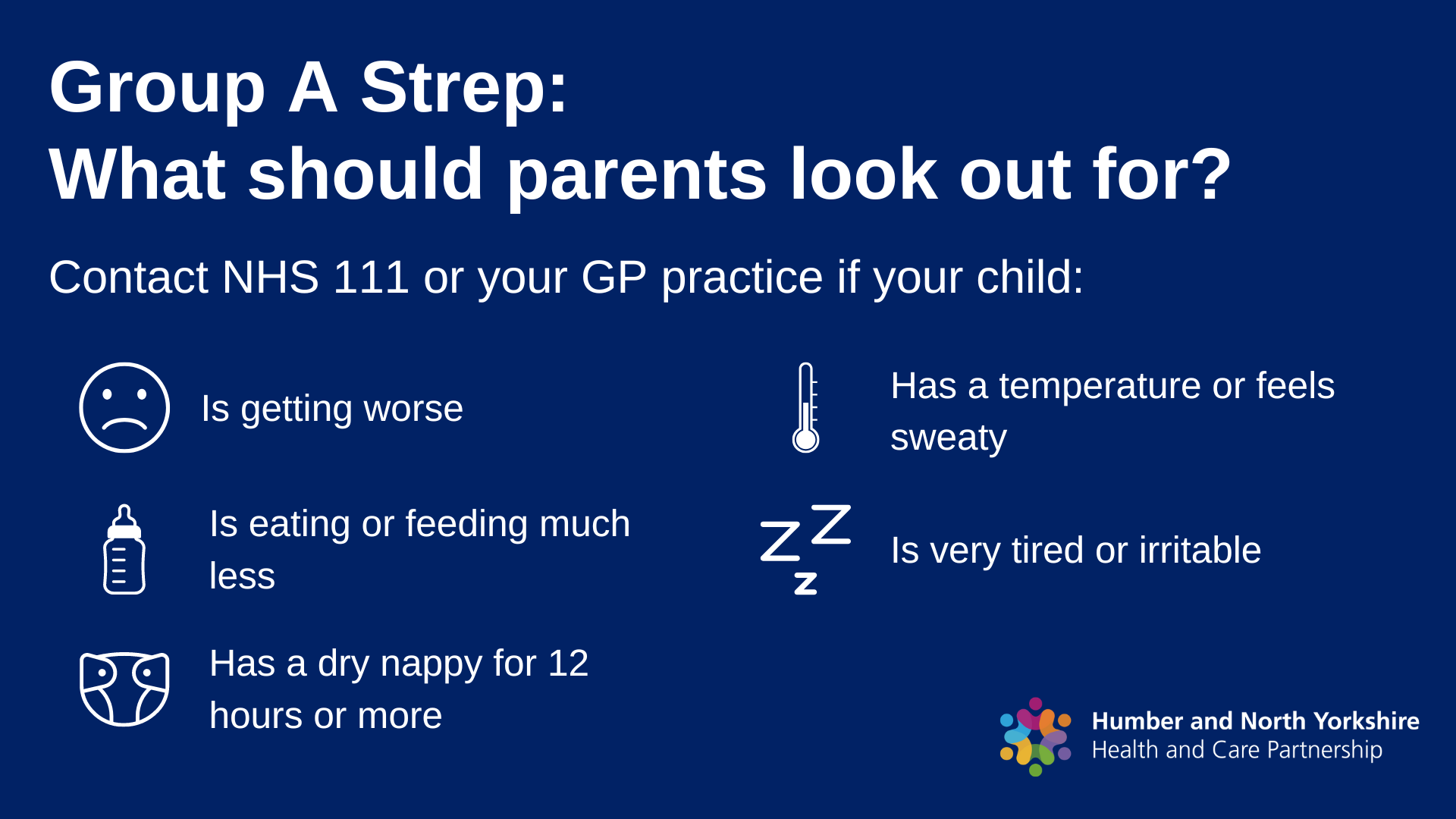
Parents should contact their GP if they feel:
- their child is getting worse
- their child is feeding or eating much less than normal
- their child has had a dry nappy for 12 hours or more or shows other signs of dehydration
- their baby is under 3 months and has a temperature of 38°C, or is older than 3 months and has a temperature of 39°C or higher
- their baby feels hotter than usual when they touch their back or chest, or feels sweaty
- their child is very tired or irritable.
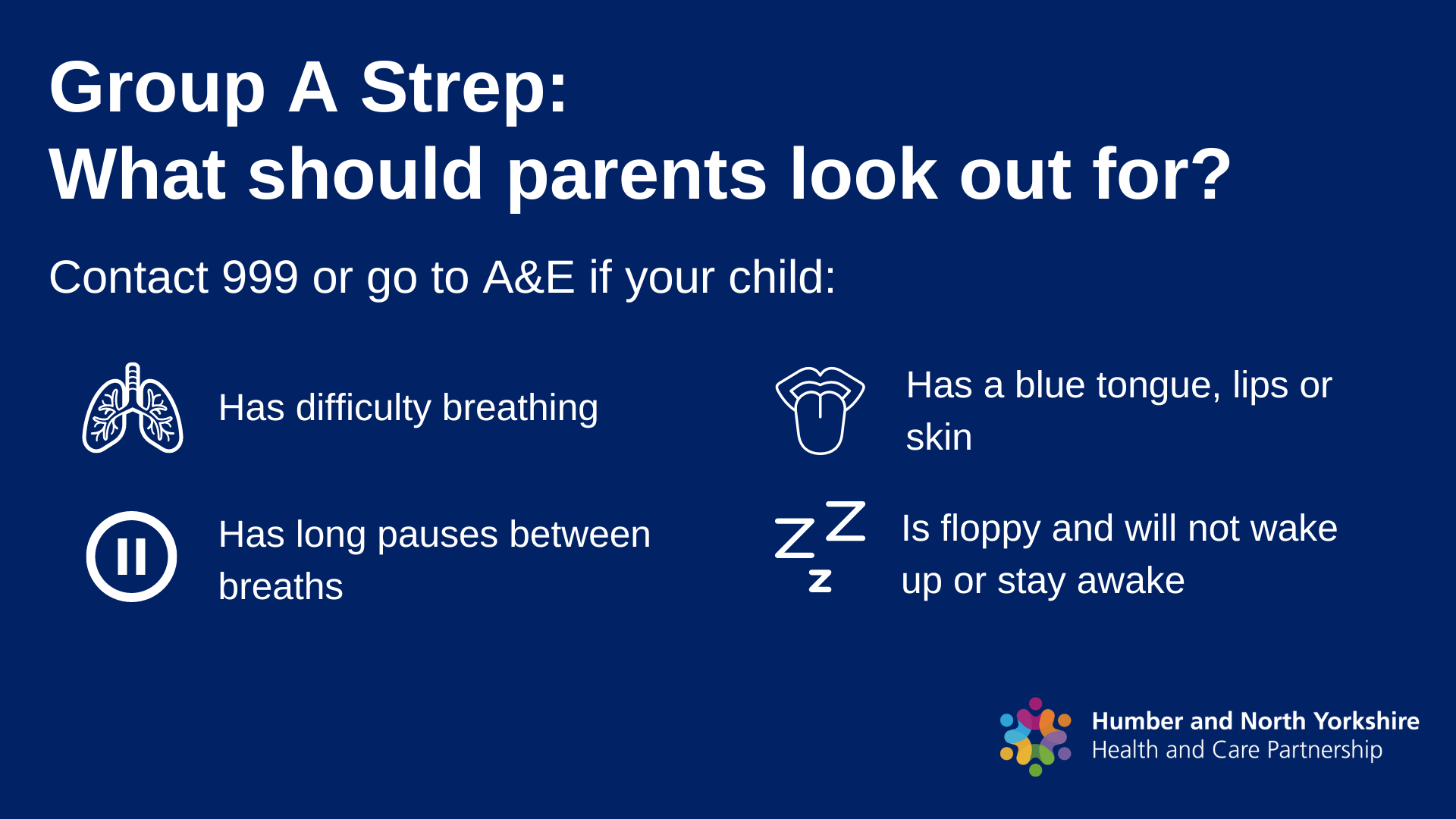
Call 999 or go to the Emergency Department if:
- your child is having difficulty breathing – you may notice grunting noises or their tummy sucking under their ribs
- there are pauses when your child breathes
- your child’s skin, tongue or lips are blue
- your child is floppy and will not wake up or stay awake.
- Don’t put off seeking help if your child continues to get worse.
Strep infections are spread by close contact with an infected person and can be passed on through coughs and sneezes.
Please consider that emergency departments and GP surgeries are very busy. If you feel that your child can stay at home or be seen elsewhere, such as a pharmacy, please do so.
Sore Throat information leaflet
Know what to look for and when to seek medical care. Go to https://humberandnorthyorkshire.org.uk/strepa/
For further information on Strep A visit: https://educationhub.blog.gov.uk/category/strep-a/
For further information on scarlet fever visit www.pha.site/ScarletFever
Nasal Spray Flu vaccination and invasive Group A Strep infection
Getting flu and other viral infections can increase the risk of invasive Group A Strep infection in the following weeks. Invasive Group A Strep infections increased during the 2009-10 flu pandemic. The flu vaccine reduces the risk of having flu and group A Strep infections at the same time therefore it reduces the chance of developing invasive Group A Strep.
We strongly recommend that children who are eligible get a flu vaccine have it – it’s the best way to protect them from serious illness. The flu vaccine for children has an excellent safety record, this includes the nasal spray given to school aged children and pre-schoolers, which has been given to millions of children in the UK and worldwide.
- There is no current evidence to suggest that the nasal spray flu vaccine given to children causes iGAS
- We know that children can become infected with invasive group A Streptococcal (iGAS) disease and influenza at the same time, causing a very severe illness. Flu and other viruses may increase the risk of iGAS, therefore we reinforce the recommendation that children who are eligible for influenza vaccination take up the offer.
- The influenza vaccines given to children have excellent safety records. This includes the nasal spray flu vaccine given to school-aged children and pre-schoolers, which has been given to millions of children in the UK and worldwide. The flu vaccination programme in England first used nasal spray vaccines in children aged 2 and 3 years and in primary schools in pilot areas in 2013 before being rolled out incrementally to older age groups over the past nine years.
- Nasal flu vaccines prevent flu in children who are vaccinated and those around them too.
- The nasal flu vaccine will help prevent influenza which can cause very severe infection.
- The nasal influenza vaccine also therefore reduces the risk of coinfection of influenza and Group A Streptococcal infections, and in turn the potential development of iGAS infections.
You may also be interested in the following UKHSA blog on Group A Strep:
https://ukhsa.blog.gov.uk/2022/12/05/group-a-strep-what-you-need-to-know/