The main symptoms of early osteoarthritis are:
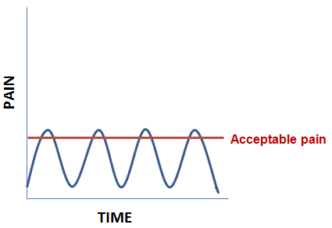
- Pain – The pain tends to be worse when you move your joint or at the end of the day. As shown on the graph, you are able to tolerate the symptoms for the majority of the time with only brief episodes where the joint is disabling
- Stiffness – Your joints may feel slightly stiff after rest, but this usually wears off quickly as you get moving
- A grating or grinding sensation (crepitus) – Your joint may creak or crunch as you move – this is normal for osteoarthritic joints – do not be afraid to move them.
- Swelling – The swelling is soft caused by extra fluid, and an sometimes be warm/ hot to the touch
- Muscle weakness – the muscles around your joint may look thin or wasted and you might experience difficulty with some activities eg: going up and down stairs
- Not being able to use your joint normally – Your joint may not move as freely or as far as normal. Sometimes it may give way because your muscles have weakened or your joint has become less stable. Exercises to strengthen your muscles can help to prevent this
Your symptoms will often vary for no clear reason – you’ll probably have good and bad spells. Some people find that changes in the weather make the pain worse, especially damp weather along with falling atmospheric pressure. Others find the pain varies depending on how active they’ve been.
Treatment options
Medications and creams can help with the arthritis pain and inflammation. Some medications can conveniently be bought “over the counter” . In order to make sure this is the right thing to do – access your local Pharmacist for advice about safe medication and creams which may help you to manage your pain/ inflammation. They will take into consideration any other medications that you may be taking and other medical conditions that you may have.
The following are Medications which are commonly recommended by the GP or Pharmacist:
- Pain killers e.g. paracetamol/ codeine
- Anti-inflammatory medications to help reduce inflammation and pain: Non -steroidal Anti-inflammatory drugs (NSAIDS) come in 2 types . the traditional medications such as Ibuprofen, Naproxen, diclofenac and the COX-2 inhibitors such as Celecoxib and Eterocoxib
- You can also get NSAID’s in creams – these are described as “topical”. They are less likely to cause upset stomachs
All qualified Pharmacists in Great Britain must be registered with the General Pharmaceutical Council (GPhC). Click here to visit the GPhC website for details about regulations and registration.
If your symptoms are concerning you then you may chose to visit the GP. The GP may request an X ray of your joint to confirm the diagnosis of Osteoarthritis. They will also advise you on appropriate medication, provide exercise information and discuss the benefits of maintaining a healthy weight
Obesity is the single most preventable contributor to Osteoarthritis for weight bearing joints. For every pound of extra body weight you may be carrying the increased loading on the knees/hips going up stairs equals 4 pounds – so for every 10 pounds overweight you are your knees will have to take 40 pounds extra load.
If you are overweight it is best to address it with a combination of healthy eating and exercise. Help with this plan can be accessed from groups such as Weight watchers, Slimming World or the local council “Fit 4 Life” program.
Fit for Life program
If you are over 18yrs and have a Body Mass Index (BMI) of 25 or above Harrogate Borough Council offers a free 12 week service called “Fit 4 Life” (funded by NYCC Public health team) which combines Nutrition and lifestyle advice with exercise sessions. These programs are offered at venues across the Harrogate district during the day and some evenings. To find an up to date timetable for Fit for Life click here.
The “Fit 4 Life” programme is made up of group sessions consisting of individual weigh-ins, physical activity and weight management advice, covering different topics each week including:
| Goal setting | Behaviour change |
| The “eat well plate” | Salt |
| Portion sizes | Benefits of physical activity |
| Eating awareness | Eating out |
| Fats Food labelling | Drinks |
Before taking part in the group session you will be required to attend an induction with the instructor. This will include a basic health check, a health questionnaire and general chat about your lifestyle.
For more information about the Fit 4 Life programme call 01423 500600 (ext. 58382)
Physical activity is the best non-drug treatment for improving pain and function in OA. While you may worry that exercising with osteoarthritis could harm your joints and cause more pain, the research has shown that people can and should exercise when they have osteoarthritis. In fact, exercise is considered the most effective non-drug treatment for reducing pain and improving movement in patients with osteoarthritis.
What exercises work best for osteoarthritis?
- Range of motion exercises can help maintain and improve the flexibility in the joints
- Aerobic/endurance exercise strengthens the heart and make the lungs more efficient. This conditioning also reduces fatigue, controls weight and builds stamina. Aerobic exercises include walking, cycling, swimming or using the elliptical machine
- Strengthening exercises help maintain and improve muscle strength. Strong muscles can support and protect joints that are affected by arthritis. You can find a list of suitable home-based exercises recommended by Arthritis Research UK by clicking here.
How do I become active?
You will benefit from most exercises although we would recommend that you do not do high impact activity i.e. running long distances on a road surface. Locally Harrogate Borough Council run exercise programs and you can find the information by emailing [email protected] or visiting the sports development section of Harrogate Borough Council Website.
If you are getting pain from your joint when walking/ weight bearing you could benefit from a walking stick. The walking stick will take some of your body weight through the hands reducing the load on the lower limb joints – there can be a 10-25% decreased load on your knees when you are using a walking stick in the hand opposite to the affected knee/hip.
There are several walking aids but in the early stages of OA a walking stick is the most appropriate. They are suitable for most people and easy to walk with.
Measuring a stick
When on the floor the handle of the stick should reach your wrist when your elbow is very slightly bent.
Using a stick
When walking with a stick use one stick in the opposite hand to the affected leg. Put the stick and the affected leg forward together.
Instruction
There are many web sites which give instructions on how to measure for a walking stick. Here’s one example:
Supply
Walking sticks can be purchased from Yorkshire Care (Forest Lane Head, Harrogate: 01423 799960) / walking shops/ garden centres/ some pharmacists/ Sports Direct etc.
Your GP could also request one to be issued from the Physiotherapy department if you need help with balance or learning to use one.
If your joint is inflamed it may be that a corticosteroid injection could help with the pain and inflammation. These injections can be done by your GP/ Physiotherapist or in the Radiology department when guidance/imaging is used.
Corticosteroid is injected to reduce the inflammation and a local anaesthetic to help with the pain. It can take up to three weeks to have full effect and the benefit can last over a year.
If you are offered an injection make sure that you plan to have a “quiet time” over the following two days to give it maximum chance to be effective.